Spinal surgery has seen transformative advancements over the past few decades, thanks to technology designed to enhance precision, reduce complications and improve patient outcomes. For patients with conditions such as herniated discs, spinal stenosis or scoliosis, these technological innovations are aiming to make spinal procedures safer and potentially more effective. Dr. Larry Davidson, a leader in minimally invasive spine surgery, highlights that cutting-edge tools are reducing the risks associated with traditional spinal surgery, allowing patients to recover faster and more comfortably.
Common Complications in Spinal Surgery
Spinal surgery, while often effective, can involve certain risks and complications that may impact recovery and outcomes. Some of the most common complications include:
Infection: Open surgery can increase the risk of postoperative infections due to large incisions and extended hospital stays.
Nerve Damage: Precision is crucial in spinal surgery to avoid nerve damage that can lead to numbness, weakness or even paralysis.
Hardware Misplacement: Improper placement of screws, rods or implants can lead to instability and require additional surgeries.
Excessive Blood Loss: Traditional open surgeries often involve significant blood loss, prolonging recovery and increasing the risk of transfusions.
By reducing these complications using advanced technology, spinal surgery has become a safer option for more patients, leading to better outcomes and enhanced quality of life.
Key Technological Advancements Reducing Complications
Several groundbreaking technologies are minimizing complications in spinal surgery by improving precision, reducing invasiveness and enhancing patient safety. Here are the most impactful innovations:
1. Robotic-Assisted Surgery
Robotic systems like the Mazor X have become integral to spinal surgeries, offering unprecedented precision and control. These systems aim to enable surgeons to perform complex procedures with high accuracy, potentially reducing the risk of human error and hardware misplacement.
How It Works: Preoperative imaging data is used to create a 3D model of the patient’s spine, allowing the surgeon to plan the procedure in detail. During surgery, the robotic arm guides instruments to precise locations, ensuring accurate placement of screws, rods and implants.
Impact on Complications: Robotic assistance reduces the risk of nerve damage and hardware misplacement, ensuring that each component is placed accurately and minimizing the chance of follow-up surgeries.
2. Advanced Imaging and Navigation Systems
Imaging and navigation technologies, such as fluoroscopy, intraoperative CT and MRI, provide surgeons with real-time guidance throughout the procedure. These systems offer continuous visualization, allowing for accurate adjustments and minimizing risks associated with blind navigation.
How It Works: Imaging systems create a detailed, real-time view of the patient’s anatomy, which is displayed on a monitor. Surgeons use this visual data to guide instruments, ensuring precision and avoiding critical structures.
Impact on Complications: Real-time imaging minimizes the risk of nerve and tissue damage, as surgeons can make accurate adjustments based on live data. This technology also reduces the chance of hardware misplacement and other complications.
3. Minimally Invasive Surgical Techniques
Minimally Invasive Spine Surgery (MISS) uses smaller incisions and specialized instruments to access the spine without cutting through large amounts of muscle or tissue. This approach is designed to minimize blood loss, lower infection risks and support a shorter recovery time while offering similar effectiveness to traditional open surgery.
How It Works: Small incisions allow the insertion of tubular retractors, through which surgical instruments are guided. MISS often involves tools like endoscopes or lasers to perform decompressions or remove damaged tissue.
Impact on Complications: Smaller incisions can mean a reduced risk of infection, lower blood loss and faster healing. Minimally invasive techniques also reduce postoperative pain and the need for opioids, promoting safer recovery.
4. Laser-Assisted Surgery
Laser technology provides a highly precise and minimally invasive way to remove or shrink damaged tissue in cases of herniated discs or spinal stenosis. Lasers offer pinpoint accuracy, which helps to
preserve healthy surrounding tissue.
How It Works: A small laser probe is inserted through a tiny incision, targeting only the affected disc tissue. The laser energy vaporizes or reduces the size of the tissue, relieving pressure on the spinal nerves.
Impact on Complications: Laser surgery may help to minimize the risks of excessive bleeding, infection and nerve impact, offering a safer alternative for patients with localized spinal issues.
5. Spinal Cord Monitoring Systems
Spinal cord monitoring systems are critical during procedures that involve complex spinal alignment or decompression. These systems track nerve activity throughout the surgery, alerting the surgeon to potential issues before they cause damage.
How It Works: Electrodes are placed on the patient’s body, monitoring electrical signals along the spinal cord. Any disruptions in these signals prompt immediate adjustments, preventing permanent nerve damage.
Impact on Complications: Real-time monitoring reduces the risk of nerve damage, ensuring that patients retain full function post-surgery and experience fewer neurological complications.
6. Artificial Intelligence (AI) in Surgical Planning
AI is becoming an essential tool in surgical planning, helping surgeons analyze patient data and optimize each step of the procedure. By examining vast amounts of data, AI can assist in predicting potential complications and customizing surgical plans to minimize risks.
How It Works: AI algorithms analyze imaging scans, previous surgical outcomes and patient medical history to develop a highly personalized and risk-averse surgical plan.
Impact on Complications: AI reduces the likelihood of complications by providing insights that help surgeons anticipate challenges and choose the safest approach tailored to each patient’s anatomy and condition.
Benefits of Technology-Enhanced Spinal Surgery for Patients
The integration of technology in spinal surgery offers numerous benefits that directly impact patient safety and outcomes. Here’s how these advancements improve the surgical experience for patients:
1. Reduced Risk of Infection and Blood Loss
Minimally invasive techniques and robotic assistance allow for smaller incisions, which may reduce infection risk and help to minimize blood loss. Patients experience less trauma during surgery, leading to faster healing and fewer hospital visits.
2. Enhanced Precision and Accuracy
Robotic and image-guided systems allow surgeons to operate with remarkable precision, ensuring that hardware placement and tissue removal are executed with accuracy. This approach may reduce the need for follow-up surgeries and support the durability of surgical outcomes.
3. Shorter Recovery Times and Less Pain
Smaller incisions, laser assistance and minimally invasive approaches mean that patients experience less postoperative pain and faster recovery. These technologies reduce the need for opioids, which can have side effects and lead to dependency.
4. Improved Long-Term Outcomes
With fewer complications and enhanced accuracy, technology-assisted procedures tend to offer better long-term outcomes. Patients are less likely to need revision surgeries and experience more durable relief from their symptoms.
5. Accessibility to High-Risk Patients
Some patients, such as older adults or those with underlying health conditions, may not be candidates for traditional open surgery. Minimally invasive and technology-enhanced techniques offer safer alternatives, expanding the pool of patients who can benefit from spinal surgery.
The Future of Technology in Spinal Surgery
As technology continues to advance, the future of spinal surgery holds exciting possibilities. Here are a few developments on the horizon:
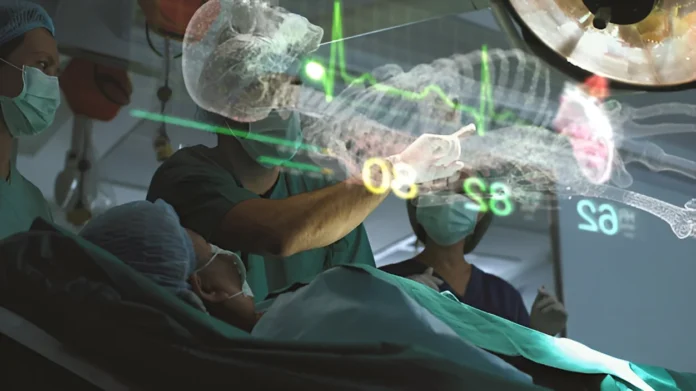
Augmented Reality (AR) Guidance: AR technology could overlay critical information directly onto the surgical field, allowing for enhanced visualization and greater accuracy.
Expanded AI Applications: AI’s role in spinal surgery could grow to include predictive analysis, helping surgeons anticipate challenges and choose the most effective treatment approaches.
A Safer, More Effective Path to Spinal Health
The role of technology in spinal surgery has redefined the possibilities for patients suffering from chronic back pain and spinal conditions. From robotic guidance and real-time imaging to AI-driven planning, these advancements are aimed at reducing complications, enhancing precision and potentially allowing for faster recovery. Dr. Larry Davidson remarks, “Spinal fusion procedures regularly involve the implantation of certain types of implants. A merger of AI and 3D printing could result in the production of an implant that uniquely serves the needs of a specific patient. Such a preparation would be done before a planned procedure based upon the imaging studies of the patient’s spine. Also, emerging minimally spinal surgical techniques have certainly changed the way that we are able to perform various types of spinal fusions. All of these innovations are aimed at allowing for an improved patient outcome and overall experience.” Spine surgery is harnessing these innovations to provide patients with potentially safer, more effective options for treating spinal conditions.